 Jason* puts his lunch tray down at an open spot at the table, at the edge of a happy, chatting gaggle of fellow sixth-graders. He takes his seat, hoping today will be better, hoping today will be the day he doesn’t end up eating alone. But it’s not to be.
Jason* puts his lunch tray down at an open spot at the table, at the edge of a happy, chatting gaggle of fellow sixth-graders. He takes his seat, hoping today will be better, hoping today will be the day he doesn’t end up eating alone. But it’s not to be.
“It wasn’t even like the other kids would talk about it,” says Dr. Leslie Walker, chief of adolescent medicine at Seattle Children’s Hospital, who observed Jason at school. “Wherever he sat, they would slowly move away from him. And he would unconsciously move to be with them again, and then they would all move away. It was really sad.”
Jason has been diagnosed with attention deficit hyperactivity disorder — ADHD — but his parents have decided not to seek treatment for him. For one thing, they don’t want him on medication. They’re also afraid treatment will stigmatize him. His behavior left untreated, Jason is sometimes random and unpredictable. He can’t sit still, often jumping up suddenly, startling those around him. The other kids don’t want to sit next to him because they never know what he will say or do. ADHD can be profoundly lonely.
That’s why some say it’s actually good news that these days, more kids than ever before are being diagnosed with the disorder. In March, a Centers for Disease Control and Prevention (CDC) report made headlines — and turned heads —with startling new data: Eleven percent of school-age children in the U.S. have been diagnosed with ADHD — about 6.4 million children between the ages of 4 and 17. That’s a 53 percent increase over the last decade.
For adolescent boys, the number is even higher: Nearly one out of every five high school-age boys has received the diagnosis.
Though these numbers probably mean that more kids like Jason are getting the treatment they desperately need, the report has sparked a national conversation over concerns that the ADHD diagnosis — and the medications used to treat it —are being vastly overused. But ask many local ADHD experts for their take, and they’ll tell you the real problem isn’t overdiagnosis.
“There’s been a lot of press recently about the higher rates of ADHD,” says Dr. Mark Stein, a national expert on ADHD who joined the staff of Seattle Children’s in April. “It raises the question: Is there overdiagnosis? And I guess my view is that yes, that’s a problem; overdiagnosis occurs. But there’s also a bigger problem: underdiagnosis and undertreatment.”
While some worry that too many of the wrong kids are being diagnosed with ADHD, Stein and others worry more about the kids who are slipping through the cracks.
“I think there’s a concern about people just missing ADHD, and defining a child’s behavior as willful or defiant or not trying hard enough,” agrees Milani Smith, Ph.D., a psychologist and the clinical director of Cadence Child & Adolescent Therapy in Kirkland, Wash. “It’s so difficult to diagnose. The tricky part about ADHD is that there is no blood test for it.”
A tough call
Accurately diagnosing ADHD is a meticulous, subjective and time-consuming process, involving extensive interviews with patients, parents and teachers — and the screening for and ruling out of a host of other conditions that often look like ADHD. “A child who is anxious can seem inattentive and distractible; a child who has a learning disability might look inattentive and distractible; a child who has a medical condition might look inattentive and distractible — and those behaviors can look a lot like ADHD,” Smith says.
Add to that the exploding new problem of kids actually faking ADHD symptoms to get their hands on the stimulants used to treat them, and it’s no wonder that teasing out the kids who truly need help for ADHD takes a lot of time — time that some pediatricians and clinicians may not have.
But catching these kids — and doing it while they’re young — is crucial, says Walker. A lot of her patients are teens who are paying a high price for undiagnosed ADHD; still others were diagnosed years ago, but, for various reasons, their parents decided not to seek treatment.
“I see kids who are failing at school, using drugs or depressed, and then we look back and find out they were diagnosed with ADHD when they were in the fourth grade, but never treated,” says Walker. “At least half of the kids I see for drug addictions have ADHD.”
With stakes this high, why are some parents choosing not to seek treatment for their children’s ADHD? For one thing, cost may be an issue: Although many insurance plans cover much of the cost of diagnosis and therapy, some of the drugs can run several hundred dollars a month, Walker says — after insurance coverage.
But beyond cost, the answer may also lie in opinions about the treatment itself, which typically involves a three-pronged approach of behavior modification, education and medication. The first two can require a level of diligence, effort and persistence that could sap the strength of a superparent; the third has increasingly drawn fire from all corners in the media.
A drugged generation?
“I had read about the number of kids that have ADHD, and I had always thought it was overdiagnosed,” says Judy, a Redmond, Wash. mom and former Microsoftie who now stays home with her two boys, ages 18 months and 7 years. “I thought, ‘Why are we drugging this whole generation of children?’ I was very biased against it.” Biased, she says, until her older boy, Daniel, began his journey with ADHD.
Judy and her husband were first tipped off that their son might need help when they brought Daniel in for an IQ test as part of a private-school application. The psychologist confirmed that Daniel is very bright — and also let them know that they should keep an eye out for possible ADHD. “Partway through kindergarten, he was having trouble, mostly socially, relating to the other kids and recognizing boundaries,” Judy says. Shortly after that, Daniel was diagnosed.
But, like Jason’s parents and many others, Judy balked at the idea of medication. “I’m very anti-medication, in general,” she says. “So my initial response was, ‘Let’s deal with everything through a behavior modification process. I do not want to drug my child.’”
The family tried to cope without medication, using behavior modification techniques such as positive reinforcement for paying attention, consequences for losing focus, progress charts and meetings with teachers. But after about three months, Judy relented. “What we found was that when these kids are in the moment, they just can’t think of consequences.”
For Judy, it was a difficult decision. “I had to let go of thinking, ‘I don’t want to have a kid on drugs.’ I had to realize that it was hurting him to not get him the help — or at least try.” After trying several medications at several dosages, Daniel has found one that appears to be working, in tandem with behavior modification. His treatment is so successful that in April, he was able to stop his regular visits to the psychologist’s office.
Smith, who treated Daniel, says Judy is part of what she sees as a growing trend in the Puget Sound area. “Parents are now much more reluctant to try medication,” she says, instead preferring to start with behavioral modification alone. “I’m not pushing medicine. But in my practice, I end up telling people, ‘When it comes to ADHD, I need to talk about the effectiveness of medicine.”
According to Stein, about 75 percent of children have a positive response to the first ADHD medication they try; about 90 percent will respond to the second or third.
It’s a pharmacological success story — but lately, it’s had a real dark side.
A ‘diversion’ epidemic
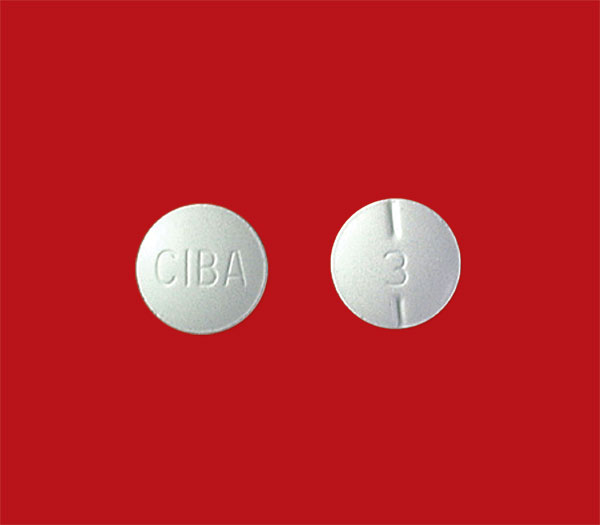
About two-thirds of the kids in the U.S. now diagnosed with ADHD receive prescriptions, according to the CDC report. The majority of drugs used to treat the symptoms of ADHD are stimulants; two of those, Ritalin and Adderall, are classified as Schedule II controlled substances — in the same class as morphine and codeine — and are considered to have a high potential for abuse.
But for any of the prescription stimulants used to treat ADHD, it may come as no surprise that “diversion”— the passing of these drugs from patient to pals for recreational use — and illicit use in general is now considered an epidemic. Beyond providing an amphetamine high, students and athletes believe the drugs also help with focus, endurance and concentration. In April, Seattle Seahawk Richard Sherman was suspended briefly from the team after he tested positive for Adderall. He told the Vancouver Sun, “About half the league takes it.”
Also in April, a New York Times story cited multiple university health systems that are implementing tough new rules about ADHD after being besieged by students faking symptoms to obtain medication to help them study. One 2008 University of Kentucky study put the number of college kids illicitly taking these drugs at about 35 percent. “I think it’s a huge epidemic on college campuses — and in some really high-intensity, high-stress high schools,” says Walker. “I see these kids all the time. They say, ‘Well, I can get ADHD meds from my friend, but I’d rather just have it from you.’ They think it’s so completely OK because so many kids are doing it.”
And it may be all for naught. “Amphetamines will make you feel like you’re on the top of the world, but research shows these kids are not performing any better than they would have done without the drugs,” Walker says. In other words, all of these kids taking all of these illicit drugs may not be seeing any real, significant benefits — they only think they are.
Which makes the risks seem particularly pointless. Though studies have shown no permanent, long-term effects of these drugs, there is evidence of an effect on growth patterns, so kids on these drugs must be carefully monitored. In the short term, the stimulants used to treat ADHD have common side effects, such as difficulty sleeping, loss of appetite, moodiness and irritability. Very rare — and very dangerous — side effects include cardiac problems, severe mood swings and hallucinations. And Walker points out another, very real danger: college kids mixing these drugs with alcohol. The drugs mask the effects of alcohol, leaving kids at risk of severe overdrinking and alcohol poisoning.
A shattering impact
With as many as one-third of U.S. college students taking illegal drugs to help them achieve, and one out of 10 children in our country diagnosed with ADHD, the staggering data has rightly generated a maelstrom of media coverage. But what the media doesn’t emphasize enough, according to Stein — what needs to be brought to the forefront — is the shattering impact of undiagnosed and untreated ADHD.
“These people are not just doing poorly in school,” he says. “They’re at risk for difficulties with the law, for health-related behaviors such as obesity, dangerous driving and accidents, and they’re especially at risk for substance abuse.”
People with untreated ADHD also have higher rates of divorce, trouble holding down jobs, and suffer from anxiety and depression. One recent study from the NYU Langone Medical Center in New York found that boys who are diagnosed with ADHD are twice as likely to be obese as adults. It’s truly a litany of misery. “In talking about treatments, you always have to weigh the benefits with the risks,” Stein says. “What is the cost of not treating this problem?”
If you suspect that your child is showing symptoms of ADHD, that’s enough reason to see your pediatrician, Stein says. “You should be worried about ADHD if you hear they’re not learning or falling behind; or you observe when they’re playing with others that they’re not able to follow play, or are very distractible; or if you’re getting very stressed and frustrated because they’re not listening.
Think of ADHD as the “terrible twos,” Stein continues. “All 2-year-olds display ADHD symptoms. When they’re 7, and they’re distractible and impulsive … talk to your child’s doctor.”
While most experts feel ADHD symptoms should surface by about age 9, the thinking on that has recently been challenged. The latest edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) expands the diagnosis to allow for symptoms that first appear much later in life, so that more adolescents and adults qualify for a diagnosis. It’s controversial, coming as it does on the heels of a national discussion about overdiagnosis.
But for parents whose kids are just starting their journey of coping with ADHD, there’s only one diagnosis that matters, one diagnosis that triggers a cascade of decisions — including whether to seek treatment, and, if so, whether to consider the use of medication. Walker says that parents should try to keep an open mind.
“It can be worth trying,” she says, “because when it does work, it is like flipping a switch for a number of kids.” One of Walker’s patients said she wanted to be a grocery bagger. “She thought that was all she’d ever be able to do. Then she got on medication, and she told me, ‘Wow, I can do more than be a grocery bagger!’”
That ninth-grader eventually went on to college, Walker says, a sweet success story that sprang from years of treatment and effort. “It can be so very profound.”
Kristen A. Russell is a Seattle-area journalist and the co-author, with Dr. Laura S. Kastner, of Wise-Minded Parenting: Seven Essentials for Raising Successful Tweens and Teens.
*Some names have been withheld or changed to protect the privacy of children.
Resources
Children and Adults with Attention-Deficit/Hyperactivity
Disorder (CHADD)
The website for this national nonprofit is packed with articles, tools, webinars and newsletters for families dealing with ADHD.
Seattle Children’s
Visit this site for background information on the causes and diagnosis of, and treatments for, ADHD. Search for “ADHD.”
National Institute of Mental Health (NIMH)
The NIMH website features a downloadable brochure of information about symptoms, causes and treatments for ADHD. You’ll find it listed under “topics” on the home page.
Dr. Russell Barkley
Dr. Smith recommends the website of noted ADHD expert Dr. Russell Barkley, which includes factsheets about ADHD and Barkley’s book, Taking Charge of ADHD.
Facts about ADHD
- Scientists aren’t sure of all of the causes of ADHD, but heredity plays a large role. A boy whose father has ADHD is 20 times more likely to have ADHD than other boys, says Stein.
- Boys are much more likely to be diagnosed with ADHD than girls; in one Mayo Clinic study, as much as three times more likely.
- According to Walker, many middle-aged people find out they have ADHD after a child’s diagnosis prompts them to get themselves tested.
- When a mom has ADHD, it’s often missed, Stein says, because symptoms tend to be “quieter” in women. This can be a real issue when her child has ADHD, since treatment often falls to the mom. Stein is currently studying whether treating the mother first can delay the onset of the need for medication for her child.
- There is no cure for ADHD, Stein says, but many people can gradually stop treatment as they get older, and most only take medication for specific periods in their lives. Medications can be especially helpful during major transition times in a child’s life — such as the shifts to middle school and high school.









